 As lactation professionals, breast milk storage guideline questions is something you will frequently navigate. Many new parents opt to pump at least occasionally, many return to work, and some will even use donor milk.
As lactation professionals, breast milk storage guideline questions is something you will frequently navigate. Many new parents opt to pump at least occasionally, many return to work, and some will even use donor milk.
Regardless of how your clients feed their baby, you are likely to be asked about human milk storage guidelines.
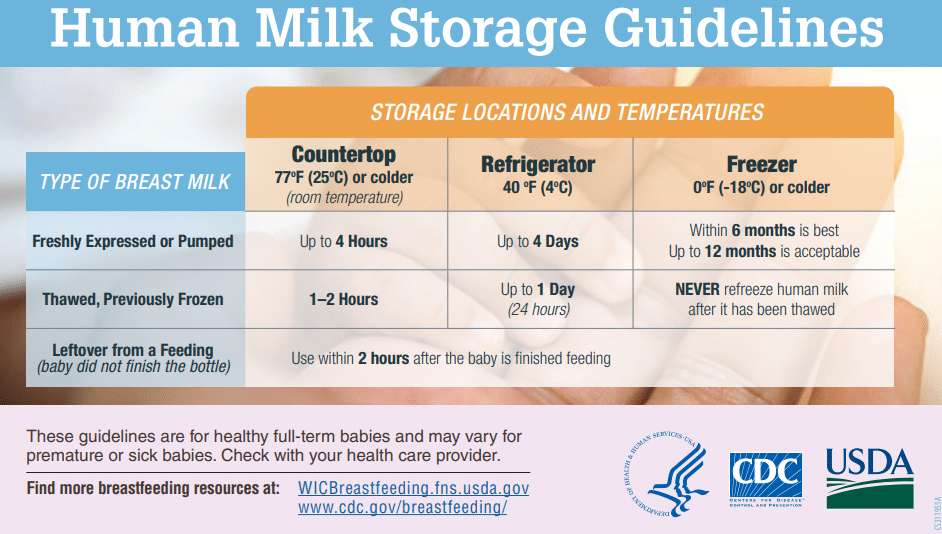
These guidelines can change over time, so it is important to keep up to date. Different sources can vary slightly. In this article, we reference the current recommendations from the Center for Disease Control (CDC) in the US. While foodborne illness via breast milk is extremely rare, it is important to follow guidelines to be safe.
Safe Storage of Breast Milk
It’s important to note that guidelines are general. There are variations in fridge and freezer temps, room temp, frequency of opening fridge and freezer, and other variables.
One rule of thumb some parents use is that if the milk smells bad, it may be bad even if it is within the ‘safe’ timeframe. It is important to remember that breast milk can smell soapy, or have other distinct smells, but it should not smell sour.
Freshly Expressed or Pumped Milk – Up to 4 hours room temp, 4 days in fridge, and ideally 6 months but up to 12 in freezer.
Thawed or Previously Frozen – 1-2 hours room temp, 1 day (24 hours) in fridge, and never refreeze thawed milk.
Once a baby feeds from the bottle, use leftover milk within 2 hours.
Before Expressing or Handling Breast Milk
Just as with any food handling, it is important to wash your hands. This is most important for outside caregivers, such as CBCs, doulas, etc., as we are more likely to bring outside germs into the home of our clients.
Parents who are pumping using a hand pump or electric pump should ensure the pieces are first washed properly according to manufacturer’s directions. After the first use, most can simply wash well with soap and water.
If they have a premature infant, or one with any medical needs, their pediatrician may advise sterilizing pumps and bottles on a regular basis. Outside of that, most parents need only sterilize as needed or according to the pump’s manufacturer.
Typical dish soap and hot water are adequate for cleaning. However, some parents prefer convenience items such as pump wipes, made for breast pump disinfectant sprays, and sterilizing bags. Before using any type of convenience products, they may want to check with their NICU or child’s doctors if there are any health concerns.
If a mother is hand expressing, it’s important she wash her hands, especially if she has any cracks or irritation on her nipples.
When using approved nipple creams and ointments, it is not necessary to clean the nipple before expressing or pumping milk.
Storing Breast Milk Safely
There are many options and containers for storing breast milk including:
- Disposable breast milk storage bags
- Disposable storage bottles, including sterile ones available in hospital settings
- Glass reusable bottles – use caution with freezing and defrosting
- Plastic reusable storage bottles
- Regular pump and feeding bottles
Before transferring milk from pump to storage containers, be sure to wash your hands. As a doula, lots of handwashing prevents germ transfer and helps reassure parents you take their safety seriously.
Be sure to label bottles and bags with the date of storage. If the milk is for a child in the hospital, or you will be storing in the fridge and not the freezer, be sure to also label with the time.
You can add milk to already stored breast milk. However, it is important you do not add body temperature milk to already cooled or frozen milk. If you have 1.5 ounces of milk in the fridge but baby typically takes 2 oz, at another pumping session you would put the expressed milk in the fridge. Once it is no longer warm, you can mix an additional ounce to the 1.5oz before keeping in fridge or moving to freezer.
If you are combining milk from multiple pumping sessions, the date and time of storage is the first session. If the milk was first pumped at 2pm, and then you add milk from 10pm, you would still need to use the milk based on a 2pm storage time. For freezing milk, as long as it’s same day, there is less concern about times.
Safe Warming And Thawing Breast Milk
One of the most important things to remember is to never microwave breast milk. While microwaves are convenient, they can cause hot spots (a burn risk) as well as alter the nutrients in the milk.
To safely thaw breast milk:
- Place in fridge overnight
- Put bottle in a cup/container of warm or lukewarm milk
- Run under lukewarm water
Once defrosted, especially in the fridge, a bottle warmer can be used. Defrosted breast milk needs to be used within 24 hours of defrosting, even once in the fridge. Never refreeze defrosted breast milk.
As a Certified Breastfeeding Counselor these are general guidelines you may use to help your clients. It is important, however, if their child is in the NICU or has any additional health concerns they follow specific guidelines from their child’s provider.